Biocomplexity Institute and Virginia Department of Health Employ Data to Support Smarter, More Informed Health Care Decision Making for the Commonwealth
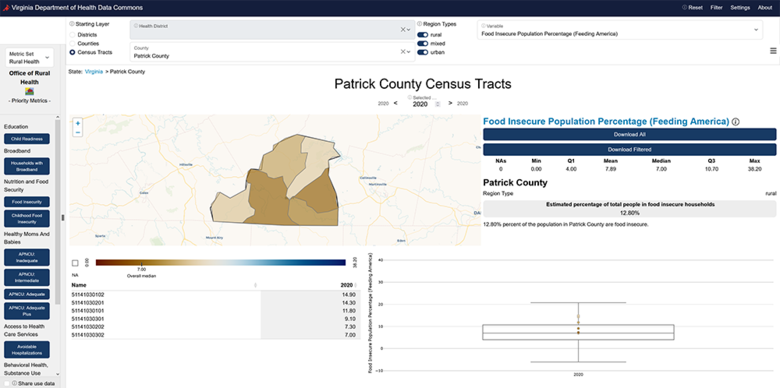
Patrick County is a rural area in central southern Virginia that over 17,600 people call home. Like in many other rural areas across the country, its residents struggled to find adequate health care services close to home. In an area where the doctor-to-patient ratio for primary care physicians is one to every 3,500 people and the only hospital closed in 2017, officials grappled with how to ensure Patrick County families had proper health care services when they needed them.
County officials reached out to the Virginia Department of Health (VDH) and the State Office of Rural Health (VA-SORH) who enlisted the UVA Biocomplexity Institute's Social and Decision Analytics Division (SDAD) for help. The Biocomplexity Institute team employed relevant demographic, health, and technology-related data to address the dearth of health care options in Patrick County. The data revealed that 76 percent of county residents lived within a 12-minute drive to an Emergency Medical Services (EMS) station. This meant that on-site and telehealth visits with medical specialists at EMS stations could be a feasible option to connect more residents to the health care they needed. The team then worked to secure funding to bring this data-informed strategy to reality.
Given the Institute's versatility in addressing a wide range of issues, the VDH and VA-SORH called on the Biocomplexity Institute once again. This time, the ask was for the Institute team to develop a dedicated health care-focused Data Commons to help bring their Virginia Rural Health Plan, which tackles a variety of public health issues for Virginia's rural areas, to life. The plan outlines seven priority metrics, ranging from education and nutrition/food security to employment and healthy moms and babies. The VDH Data Commons enables public health officials, policy makers, researchers, and others the ability to study and monitor the seven priority areas and their respective metrics in a public-facing interactive dashboard.
Since fall 2021, SDAD has led a cross-disciplinary team in developing the Social Impact Data Commons, an open-source curated knowledge repository that co-locates data from a variety of sources, including public datasets, administrative records, and private entities.
The Data Commons also integrates analytical tools that enable local government and community leaders to access, review, and make decisions based on real-time data. Over the last couple of years, the Social Impact Data Commons has enabled officials in the Washington, D.C. metropolitan region to tackle a broad range of issues ranging from broadband access and food security to business district health and longevity.
In building the VDH Data Commons, the SDAD team leveraged its work on the Social Impact Data Commons as a foundation. Now, with access to more data sources, the team could build out verified, retrospective datasets for all seven priority health-related metrics. They created datasets dating as far back as 2015, enabling users to track how geographies have fared in these priority areas over time. According to Aaron Schroeder, principal investigator and research associate professor in SDAD, "this is the first time the public has had access to historical health-related data over time for geographies throughout the Commonwealth."
Further, in partnership with the VDH Office of Health Equity, the SDAD team expanded the project to integrate the Health Opportunity Index (HOI) – a numeric figure based on 14 indices and more than 30 variables that are combined to give broad insight into the overall opportunity Virginians in specific geographic areas have to live long and healthy lives. HOI figures can be viewed by district, county, or census tracts in the dashboard.
"We were initially looking to use some of the existing indices already out there, but what was available wasn't actionable and did not provide the opportunity to compare data in a given location over time," said Rexford Anson-Dwamena, social epidemiologist and spatial analyst for the VDH Office of Health Equity who developed the HOI. "We talked to stakeholders and policymakers to find out what variables affect people in their communities and put these into four HOI components measuring Economic Opportunity, Built Environment, Consumer Opportunity, and Social Impact."
"When we're talking about health opportunity, we're talking about issues across public health," said Schroeder. "Yes, that includes access to care, but it also includes all the things that contribute to public health that need to be addressed. That's what the HOI is doing. It combines a variety of factors such as economics, infrastructure, social involvement, consumer opportunity, education – they all add up to demonstrate the places where health is really good or really bad because of all these factors."
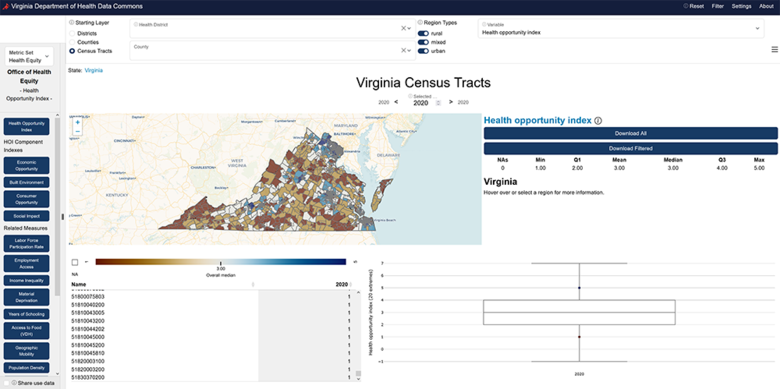
The HOI has already had widespread application throughout the Commonwealth. Users have included Virginia's health districts, numerous hospitals, nonprofits, health agencies, and graduate students, among others.
"The HOI has been highly useful for a variety of practical purposes," Anson-Dwamena said. "It's been used to place doctors in areas where there were shortages, to install streetlights in locations where there have been a number of fatalities, to identify areas where people with diabetes were repeatedly going to the ER so they could be provided with better diabetes-related education…the utility for the HOI is endless."
Joel Thurston, senior scientist and research manager in SDAD, said the VDH Data Commons enables users to see not only how Virginia's communities have fared health-wise historically, it can also help project how they will do in future years.
"This is our first foray with the Data Commons in integrating a forward-looking piece and adding projections," he said. "Now that we've gone back and put together verified datasets for the priority metrics as far back as we can, we can create Health Opportunity Indexes for each of those years, see how the different geographies have done over time, and based on the data, where they may be headed in the future."
"We can tie the HOI methodology that VDH has developed combining the 14 different indices and dozens of underlying variables together in a way that predicts life expectancy for people in different communities across the Commonwealth. By identifying the way each index or factor contributes to these projects, we can help decision makers understand the influences at work in a given population and make data-driven decisions," Thurston continued. "There is potential for this implementation of the HOI to serve as a model for other states and communities across the country."
The VDH Data Commons was built to be replicated and scaled, Schroeder explains. "The way it was built was intentional, using a lightweight JavaScript front end that you can run anywhere. It's all open source, so anyone can take the software, make their own version, and host it. We developed it to be as low cost and performance oriented as possible."
Looking ahead, the SDAD team has plans to continue its work to enable forward-looking projections in the VDH Data Commons and combine all the aggregated data to enable additional public-facing capabilities such as a life expectancy calculator.
"Our goal is for community leaders and officials to have open access to current, reliable data for more informed decision making around issues that affect people's lives, not only in Virginia, but in communities everywhere," said Schroeder.